Medical disclaimer: This article is for education only. It isn’t medical advice, diagnosis, or treatment. If you think you may have a substance use disorder (alcohol, drugs, or prescription misuse), talk to a qualified health professional.
Need help right now? SAMHSA’s National Helpline is free, confidential, available 24/7, 365 days a year (English/Spanish): 1‑800‑662‑HELP (4357).
Table of Contents
If you’re here, the storm is probably already inside the house.
Not the poetic kind. The real kind: sleep gone, appetite gone, phone full of unanswered texts, and a brain that keeps promising “tomorrow” while it steals another week. You’re not reading this because you’re curious. You’re reading this because you’re trying to figure out what kind of help exists—and which kind you need before you become collateral damage.
This isn’t a brochure.
This is a battlefield map in plain English: types of addiction treatment programs—what they’re for, how they connect, and how people get hurt when they treat detox like a war plan.
We’re going to break down inpatient vs outpatient, PHP vs IOP, and where detox actually fits—so you don’t guess wrong and pay for it.
The first truth: addiction treatment is not one thing
Most people ask, “Which program should I pick?” like they’re choosing a gym membership.
But addiction isn’t a gym problem. It’s a survival problem. That’s why treatment has levels of care—because people arrive with different risks:
- Some are medically unsafe to stop at home.
- Some are safe to stop but can’t stay stopped without structure.
- Some can do outpatient—but only if the home environment isn’t a minefield.
- Some need long-term support because relapse risk doesn’t vanish just because you hit Day 30.
So instead of “one right program,” think: the right intensity for right now, plus a plan for what happens next.
Because the most dangerous time is often not the first day you quit.
It’s the gap after the first win—when the storm quiets down just enough for you to think you’re fine, and you walk back into the same life with the same triggers and no reinforcements.
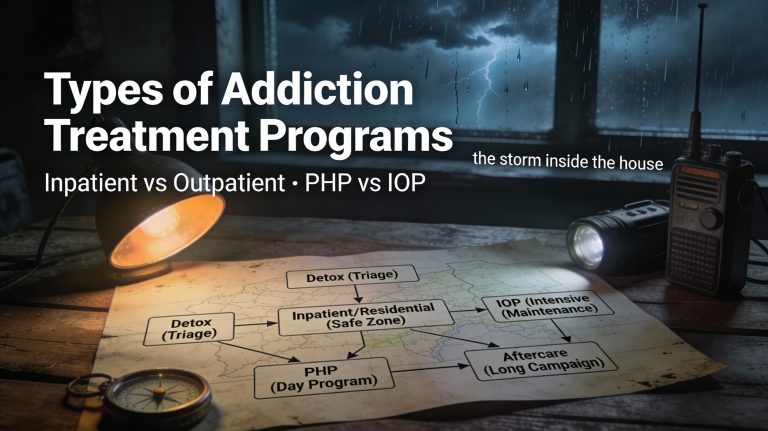
The battlefield model: triage → stabilization → training → long campaign
Here’s the cleanest way to understand treatment without drowning in acronyms.
1) Triage (Detox / withdrawal management)
This is “stop the bleeding.”
It’s about acute withdrawal, medical monitoring, stabilization, and not dying from a decision that was supposed to save you.
2) Stabilization (Inpatient / residential / sometimes PHP)
This is “get you out of the blast zone.”
It’s about structure, distance from access, support while your nervous system is raw, and building enough routine that you can function without the substance as your crutch.
3) Training (PHP / IOP / outpatient therapy)
This is “learn how to live under pressure.”
It’s where you practice coping skills, relapse prevention, emotional regulation, and honest accountability while life keeps trying to knock you sideways.
4) Long campaign (Continuing care + recovery supports)
This is “keep your position.”
It’s staying connected long enough for your brain and habits to change—not just for two good weeks, but for the months where boredom, stress, and ego come back to collect.
That’s the war plan.
Now let’s translate the program types.
The quick definitions (no brochure language)
When people search “types of addiction treatment programs,” they’re usually staring at a list like:
Detox. Inpatient. Residential. PHP. IOP. OP. MAT. Aftercare. Sober living. Therapy. Groups.
Here’s what those mean in plain English:
- Detox (withdrawal management): Medical stabilization when stopping is risky or withdrawal is already happening.
- Inpatient (hospital-level): 24/7 medical and psychiatric care; you stay overnight.
- Residential rehab: You live at the facility; structured recovery environment.
- PHP (Partial Hospitalization Program): High-structure daytime treatment; you go home at night.
- IOP (Intensive Outpatient Program): Structured treatment multiple days/week; you live at home.
- Outpatient (standard OP): Therapy/groups/med management weekly or a few times/week; you live at home.
- Medication treatment (often called MAT): Meds that reduce cravings/withdrawal and lower relapse risk; paired with counseling/support.
- Sober living / recovery housing: A stable, substance-free living environment with accountability; often used between residential and outpatient.
- Continuing care / aftercare: Ongoing support after a higher level of care; relapse prevention, check-ins, groups, therapy.
You don’t need to memorize acronyms.
You need to answer one brutal question at each step:
Am I safe where I’m sleeping tonight—and if not, what level of structure fixes that?
Detox: the triage tent (necessary, but not treatment by itself)
Detox is often the first door because withdrawal is loud. It screams. It convinces you that if you can just get through this, you’ll be fine.
But detox is not the war.
Detox is triage: evaluation, stabilization, and—this part matters—entry into ongoing treatment. If detox ends with you dumped back into the same environment with no next-step scheduled, you didn’t get a plan. You got an intermission.
Who detox is for
Detox is for people who:
- Are at risk of dangerous withdrawal (or don’t know if they are).
- Have tried to stop and got slammed by symptoms.
- Are medically fragile.
- Are using in a way that makes “just quit” unsafe.
The detox-only trap
The detox-only trap looks like this:
You suffer. You stabilize. You feel human again. You go home. You tell yourself, “I proved I can stop.” Then the storm returns—cravings, insomnia, anxiety, your old routines—and you use again.
Not because you’re broken.
Because you tried to win a war with a bandage.
If you want the full detox vs rehab vs PHP vs IOP chooser guide with a decision tree, link to your existing post here:
Detox vs Rehab vs PHP vs IOP (Which Level of Care Fits Me Best)
Inpatient vs outpatient: protected zone vs real-world missions
This is a major SEO battleground for you: inpatient vs outpatient.
People ask it like it’s about convenience.
It’s not.
It’s about whether your current condition can survive freedom.
Inpatient: “You do not get to be alone right now”
Inpatient is 24/7 care. You stay overnight. Medical staff are there. It’s used when:
- Withdrawal risk is high.
- Psychiatric symptoms are severe.
- Safety is a daily question.
- You cannot be trusted with access—because cravings are commanding your hands.
War translation: inpatient is being pulled off the front line because your odds of getting taken out are too high.
Outpatient: “You can go home—but the war comes with you”
Outpatient means you attend treatment and leave the same day. That includes:
- Standard outpatient (weekly-ish care).
- Intensive outpatient (IOP).
- Partial hospitalization (PHP).
War translation: outpatient is training and treatment while you still live in the world that taught you to use.
Outpatient can work beautifully—if your home base is stable.
Outpatient can also fail spectacularly—if your home base is actively hostile.
Residential rehab: base camp for rebuilding (when home is enemy territory)
Residential is when you live at the program. It’s not just “intense therapy.” It’s environment control.
Because sometimes the problem isn’t only cravings. It’s access, people, places, patterns, and the fact that your “normal life” is soaked in triggers.
Residential is often the right move when:
- Going home tonight means you will use.
- You’re surrounded by active use.
- You keep trying outpatient + willpower and keep disappearing.
- Your mental health is unstable and structure is the difference between safety and disaster.
War translation: residential is base camp—sleep, meals, routine, accountability, skill-building, and distance from the supply line of your addiction.
PHP vs IOP (IOP vs PHP): the difference in plain English
This keyword pair matters: IOP vs PHP.
Here’s the simple difference:
- PHP = more hours, more structure, more contact. Often most weekdays for many hours/day.
- IOP = fewer hours than PHP, still structured, multiple days/week. Commonly around 9+ hours/week, but programs vary.
Both are outpatient (you go home). That’s the blessing and the danger.
PHP: daytime deployment, nights back at base
PHP is heavy structure without living onsite. It’s for people who need:
- Near-daily support.
- A full schedule that keeps them from spiraling.
- A step-down from residential while still protected.
- A step-up from IOP because IOP isn’t holding the line.
PHP works best when:
- Nights at home won’t become relapse time.
- You have a safe place to sleep.
- You can show up consistently.
PHP struggles when:
- Nights are where you use.
- Home is unstable, unsafe, or actively triggering.
- You don’t have transportation/childcare/work flexibility.
War translation: PHP is being in the unit all day. Nightfall is the risk—because that’s when you’re alone with your thoughts and your old habits.
IOP: structured training while real life swings at you
IOP is the bridge between “weekly therapy” and “living in treatment.” It’s for people who:
- Need accountability multiple times a week.
- Need skills and support under real-life conditions.
- Can stay safe outside a facility, even if it’s hard.
IOP is a strong fit when:
- You can reliably attend.
- You have at least one safe person or safe place.
- You need structure because your brain rewrites history when you’re alone.
IOP is usually not enough when:
- Your home is an active using environment.
- You’re relapsing constantly and hiding it.
- You’re trying to stop without an assessment and withdrawal risk may be high.
War translation: IOP is drills and training while bullets still fly. It’s where you learn what triggers you in real time and bring it back to the unit for strategy.
Standard outpatient: the long, quiet work that keeps you alive
Outpatient (standard) is usually lower hours: weekly therapy, groups, check-ins, medication management, and ongoing relapse prevention.
People underestimate it because it doesn’t look dramatic.
But outpatient is where life actually changes—because it’s done inside the real world: jobs, bills, relationships, boredom, grief, and the random Tuesday where you feel “fine” and decide you don’t need anything anymore.
War translation: outpatient is maintenance patrols. You don’t win glory. You keep your position.
Medication (MAT): armor, not a moral failure
Some people hear “medication” and think:
- “That’s cheating.”
- “That’s trading one addiction for another.”
- “I should do this on willpower.”
That purity myth kills people.
Medication can reduce cravings and withdrawal and lower relapse risk, especially when paired with counseling and structure. It doesn’t magically fix your life, but it can stop the physiological ambush long enough for you to learn skills and rebuild.
War translation: meds are armor and air support. They don’t make you brave. They keep you alive.
Sober living / recovery housing: changing the terrain
Sometimes the right program isn’t enough because the place you sleep is the trigger.
Sober living (recovery housing) can be a powerful middle ground:
- More freedom than residential.
- More structure than “back home.”
- Built-in accountability.
- A culture of recovery around you instead of a culture of relapse.
War translation: it’s a forward operating base. You can still run missions (work, outpatient), but you’re not sleeping in enemy territory.
Therapy and groups: the weapons inside the program
A program is a container. What matters is what happens inside it.
In plain English, most effective treatment includes:
- Skills training (coping, cravings, emotion regulation, relapse prevention).
- Behavior change work (routines, boundaries, accountability).
- Mental health care (depression, anxiety, trauma, bipolar, ADHD—whatever is fueling the engine).
- Group support (because addiction thrives in isolation).
War translation: therapy is where you learn the enemy’s tactics. Group is where you stop fighting alone.
The handoff problem: where people fall through the gap
Here’s a hard truth: people can survive detox and still die in the weeks after.
Because the handoff fails.
A real system has planned transitions:
- Detox → residential or PHP (not “figure it out later”)
- Residential → PHP/IOP + housing plan
- PHP → IOP → outpatient
- Outpatient → continuing care + peer support
When a program can’t answer “What happens next?” you’re not looking at a plan. You’re looking at a cliff.
War translation: the gap between units is where the enemy picks you off.
Which one do I choose? (a brutal, useful decision guide)
You already have a decision tree in your existing article. Here we keep this one broader—focused on program families and safety.
Answer like you’re under oath:
- If I stop, could I get medically unsafe—or do I not know?
If yes/unsure: start with an assessment for detox/withdrawal management. - If I go home tonight, will I use?
If yes: residential/inpatient is the straight answer (or sober living + very high structure, depending on risk). - If I go home tonight, will I be safe but miserable and unstable?
If yes: PHP or IOP depending on how much structure you need. - Do I have a next-step plan already scheduled?
If no: you’re exposed. Fix the handoff before you discharge from anything. - Is my home a recovery environment or a relapse environment?
If relapse environment: outpatient may not be enough unless housing changes.
This isn’t about “deserving” a level of care.
It’s about matching the intensity to the threat.
Red flags (sales language that gets people killed)
You already nailed several in your existing post. Here’s the expanded version for all program types:
- “Detox is all you need.”
- No step-down plan, no scheduled handoff.
- Dodging questions about hours, staffing, medication policies, discharge planning.
- Miracle language (“guaranteed cure”).
- Pressure to commit without an assessment.
- Shaming you for asking about costs, insurance, or alternatives.
War translation: if they won’t show you the map, they’re not leading you—they’re selling you.
Scripts you can steal (because panic kills plans)
Script: calling a program
“Hi. I’m trying to stop using. I need an assessment for the right level of care—detox, residential/inpatient, PHP, IOP, or outpatient. I’m not looking for detox-only with no follow-up plan. What does the step-down plan look like, and can it be scheduled before discharge?”
Script: calling a safe person
“I’m trying to stop. I’m scared and I’m not safe alone. Can you stay with me or stay on the phone while I line up help?”
Script: when shame shows up
“I’m not asking for permission to be sick. I’m asking for help to get better.”
The long-term war plan (what happens after “treatment ends”)
The most common relapse story isn’t “treatment didn’t work.”
It’s “treatment ended and life kept happening.”
A real long-term plan includes:
- Continuing therapy and/or groups.
- Recovery community/peer support.
- Medication management if needed.
- Sleep, nutrition, movement (boring but lethal to relapse).
- A relapse response plan (not a shame spiral).
- Boundaries with people/places that keep pulling you back.
War translation: you don’t win by surviving one battle.
You win by building supply lines and reinforcements and staying connected long enough for the brain to stop negotiating with death.
Where to start if you’re overwhelmed
If you’re overwhelmed, don’t start with the perfect plan.
Start with the next right step:
- If you might be medically unsafe to stop: get an assessment for detox/withdrawal management.
- If home is the trigger and you’ll use tonight: residential/inpatient (or at minimum remove yourself and get help immediately).
- If you can be safe at home but you’re unstable: PHP or IOP.
- If you’re stable but relapse keeps creeping in: step up your structure before it becomes a disaster.
And if you just need a fast, brutal chooser guide for detox vs rehab vs PHP vs IOP, go here:
Detox vs Rehab vs PHP vs IOP (Which Level of Care Fits Me Best)
If the Storm Has Turned Bad
- SAMHSA National Helpline: 1-800-662-HELP (4357) — free, confidential, 24/7/365 treatment referral and information for individuals and families; available in English and Spanish.
- FindTreatment.gov: a directory for finding treatment options in the U.S.
- If you’re in crisis or thinking about hurting yourself, call or text 988 (U.S.) for free, confidential, 24/7 support from the 988 Suicide & Crisis Lifeline.
Some links below are affiliate links—if you click or decide to use their service, this site may earn a small commission at no extra cost to you. It helps keep the lights on, and only services worth recommending get linked.
- Talkspace provides virtual therapy (and also offers psychiatry services on its platform), so support can happen from a phone or computer instead of an office visit.
- Online-Therapy.com is a CBT-focused online therapy platform that combines a self-guided program (sections + worksheets) with therapist support, including messaging and optional live sessions depending on subscription level.
- Brightside offers an online Intensive Outpatient Program (IOP) for substance use disorder, built around a weekly schedule that includes group therapy, individual therapy, and psychiatry/med consults as needed.
Build Your Storm Shelter
- Early Recovery Guide – Start here (Our Foundation)
- Relapse Prevention Plan (because when rebuilding, stress is real).
- Boundaries (we need protection, not walls)
- Rebuilding Life After Addiction (built upon our foundation)
Stormfront Dispatches
- One Year Clean
- How to Choose a Rehab Without Getting Exploited (Stormborn’s Field Guide)
- Types of Addiction Treatment Programs: Inpatient vs Outpatient, PHP vs IOP
- Am I Addicted? The Storm Test (11 Signs of Substance Use Disorder + What to Do Next)
- Cravings Plan: Twenty Minute Fight in the Teeth of the Storm